Awake surgery: Surgeons perform, patients … talk and sing
20/07/2020 07:25
Vietnamese medicine has many new or improved surgical techniques, developed from existing techniques, which effectively treat patients with complex, difficult-to-access diseases.

Dr. Ngo Manh Hung explained why it is necessary to connect circuit for treatment – Photo: L.ANH
Surgical through natural orifices
Ms. H.B., 37 years old, in Long Bien (Hanoi), suddenly blurred in one eye and almost lost the other one. The findings of MRI showed that she had pituitary tumor, the tumor grew bigger and affected her vision.
Ms. B. had surgery to get a pituitary tumor about 3cm in size through nose at Viet Duc University Hospital. Only 1 day after surgery, her eyesight has regained somewhat, 5 days after surgery she looks wider and 6 days after surgery she is discharged from the hospital.
“Since leaving the hospital, the ability to look has increased every day, the vision is wider, and is close to before,” Ms. B. said.
Dr. Nguyen Thanh Xuan – Deputy Chief of Department of Neurosurgery I (Viet Duc University Hospital) – explained this technique is performed by putting medical equipment through nose and sinus sawing to bring the device to near tumor, combined with the navigation system helps device accurately find tumor, remove the tumor out, also through nose.
Nasal incision is also used to take pituitary tumors, meningiomas, and pharyngeal tumors. The oral route – another “natural” orifice – is used to remove tumors in the lower position of brain, such as skull base …
Also, at Viet Duc University Hospital, a patient over 60 years old, diabetic, recently manifested round swollen face (like someone who overdosed of corticosteroids and had water retention), stretched skin … but did not know this was early signs of pituitary adenoma to treat at the right time.
“We had surgery to take the tumor out through nose, patient has recovered, was transferred to Bach Mai Hospital to continue treatment of diabetes,” Dr. Xuan said.
Doctors can now perform laparoscopic surgery to remove the tumor from 5cm back through natural route. However, whether or not the tumor will recur depends on whether tumor is removed at surgery and patient’s location. However, for patients who have been treated, the effect is significant.
Due to the specialty of surgical site, doctors use special materials to heal tumor, such as using nasal mucosa or thigh fat to attach open positions to tumor. “The places that are glued just a few days later are transformed by the body to fix the opening. The human body is so magical” said Dr. Xuan.
Dr. Xuan said when he was young, he did not imagine that one day he would perform surgery through nose and mouth, but the development of medical technology and the support of device led to very new treatments, very effective.
Compared with conventional methods (open surgery), the surgery through natural orifice is limited to open brain to find tumors, the location to open very small, faster healing time and softer surgery. This is significant when 90% of pituitary tumors can undergo laparoscopic surgery via a natural opening.
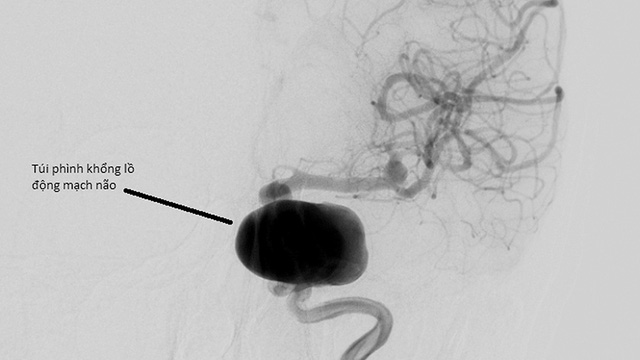
Picture: A large aneurysm of brain artery, in order to cover this aneurysm costs VND 500 – 600 million: CTV
However, according to Dr. Xuan, there are not many surgeons who can perform this method, only those who are proficient in laparoscopic, microsurgery and many other techniques with the help of equipment can do it.
Patient can hear the sound of skull drill during surgery
There have been a number of brain surgeries that have been operated by “awakening surgery” at Viet Duc University Hospital over time. One of the patients performing this technique is Mr. C.Q.C., 56 years old, in Dong Hoi (Quang Binh).
Mr. C. said that near the time of surgery, he started to have a numb feeling in his left hand, it was difficult to move, he could barely grasp things, sometimes walked or staggered.
Doctors discovered Mr. C. had a tumor of 2.3 x 3.6cm in the brain, recommended him to “wake up surgery” and the patient agreed. Within 3 hours of surgery, patient awoke up to 2/3 of the time (beginning of the surgery), still spoke and sang.
These symptoms are intended to help alert the doctor if cutting into the speech or motor nerves. Contrary to the many fearful cases of being awake by brain surgery, Mr. C. said he was “interacting with the doctor” and felt excited about this.
After the operation, Mr. C. said that he was able to immediately remind the fingers in his left hand that had been numb and that he was able to hold his chopsticks. Normally he is left-handed, when he becomes ill, his left hand becomes helpless, unable to handle it.
Dr. Dong Van He, Vice director of Viet Duc University Hospital – an experienced surgeon of this method, said that this is a new surgical technique, requiring patient’s courage because when patient was still awake, I heard the sound of skull drill, the clipping of tools.
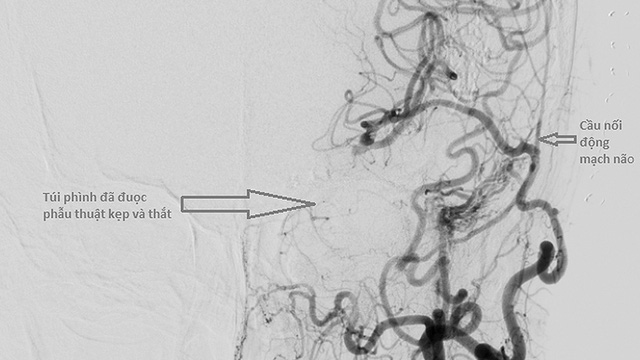
Connect an external circuit inside, create a new path to bring blood to the brain (cost tens of million), then tie the other bag away – Picture: CTV
Surgery for vascular anastomosis
Dr. Ngo Manh Hung – Deputy Chief of Department of Neurosurgery II (Viet Duc University Hospital) – said that vascular surgery is an indication that can be used to intervene in patients with cerebral aneurysms or embolism, risk of catastrophe.
Previously, doctors had to cut an enlarged part and reconnect, intervene from the outside or intervene from the inside by blocking the blood vessels. These are the two most common ways. But for patients with multiple aneurysms or aneurysms, neither of these methods is worthwhile, while still removing the aneurysm and preserving blood vessels.
“At that time, we will connect the circuit, both for professional management and to reduce the cost of treatment due to the large bulge pouch, which can cost hundreds of millions Dong. Treatment circuitry is a lifesaver option. Patients with cerebral ischemia progresses, the vessels in the brain become narrower causing brain anemia, the risk of stroke, causing weakness, paralysis, impaired memory, epilepsy …
At that time, we also applied the method of connecting cerebral vessels, increasing blood to the brain, but this designation less than solving the giant aneurysm as above” Dr. Hung said.
Another indication is now more known: the disease has a mechanism similar to progressive brain ischemia, mainly seen in young people. Because of the narrowing of the artery, the body produces another new circuit that travels to the ischemic area.
In the process, the blood vessels are weak so there is a risk of rupture. Then there were two cases: the first was found in children, because the area needed a lot of blood but this vessel was still weak (because patient was a child) and could burst.
The second case is seen in older people, due to insufficient blood vessels leading to a situation in which the new vessel does not provide enough blood flow leading to stroke. When the surgeon provides enough blood, the neovascularization will gradually weaken, lose, and the risk to patient will be less.
“The vascular surgery has been done at Viet Duc University Hospital for many years but in the past, under difficult conditions, materials such as extremely small sizes for cerebral sutures were not enough to perform regularly. Recently we continue to implement this method, when conditions are more favorable” Dr. Hung said.
This technique requires the coordination of many doctors (cardiologists, neurosurgeons), consisting of two phases.
Stage 1, surgeons take a vein in the leg, connect from the neck and then thread under the skin, connecting to a vein in the brain. The cardiologist will take the pulse in the leg, neurosurgeon will take the next step to connect neck with brain. Stage 2 is to take a vein under scalp, open it and plug it straight into a vein in the brain.
The size of the brain blood vessel is about 1mm, when connecting the doctor, the stitches will be sewn with very small thread (equivalent to type 4.0, the higher this number, the smaller the thread size). Particularly for cerebrovascular sutures is only 10.0.
Few years ago, the world rarely used this method and replaced with vascular intervention, but after a while found that vascular intervention had a high rate of recurrence, they began to return to the method of vascular connection.
Previously when the brain was interfered, patients were very afraid of affecting their memories and quality of life later.
However, Dr. Hung affirmed: “Connecting vessels does not affect the memory, as connecting vessels needed us to “lock” for not having intravascular blood (such as lock plumbing). Normally we connect a hook for 13 minutes with 12-14 stitches, which means 1 minute for a stitch.
In general, the world is equivalent to this number, in about 15 minutes, this is a golden time. My teacher in Japan can do it in 11 minutes. In order to make anastomosis we have to stop supplying blood to that blood vessel; Theoretically, the shorter the time, the sooner the blood is refilled, the less complications”.

Doctor requires patient H.B count fingers in order to evaluate the recovery of the eye – Picture: Lan Anh